A free Narcan Emergency Rescue Kit provided to employees who participated in Narcan/Naloxone training.
In August 2024, 29 PSTA staff gathered in the auditorium for an hour-and-a-half class on Narcan, a drug with the power to “pause” fatal opioid poisonings until help can arrive. Although the August class was the second one given to staff, it would mark the beginning of PSTA’s new effort to stock every bus and bus terminal with Narcan.
But before we dive into PSTA’s new initiative, we need to understand what Narcan/Naloxone is, why it’s needed, and how anyone can experience opioid poisoning, not just people with substance use disorders.
What is Narcan/Naloxone?
 A box of Narcan nasal spray.
A box of Narcan nasal spray.
(Courtesy of Narcan.com)
Narcan is the brand name for generic Naloxone, which is an opioid antagonist used to temporarily reverse the life-threatening effects of an opioid emergency. The drug works by blocking opioids from attaching to the brain’s opioid receptors. Narcan also replaces opioids already bound to the brain’s receptors, essentially kicking them out and temporarily halting the symptoms of an opioid poisoning emergency.
Naloxone was first patented back in 1961, with the Food and Drug Administration (FDA) approving it for opioid abuse treatment in 1971. In the 80s and 90s, only emergency medical personnel and hospital staff had access to this life-saving remedy. While it was available via prescription, people seeking Narcan/Naloxone faced high co-pays and stigma from pharmacies due to an overall lack of understanding of the drug.
It wouldn’t be until 2023 when the FDA finally approved the first over-the-counter Naloxone product, the nasal spray Narcan. Naloxone comes in a few product types: injectable via syringe, auto-injectable (similar to an EpiPen), and one-time-use nasal spray. The nasal spray is by far the easiest, without the need for safe needle disposal.
The approval of an over-the-counter Naloxone option was sorely needed, as opioid-related deaths have continued to skyrocket year after year since the late 1990s. With easier access and improved education for Narcan/Naloxone, everyday people now have access to an easy-to-use tool that saves lives.
The best part? Narcan is safe to use for people of all ages or medical backgrounds, even if they are not experiencing opioid poisoning. Administering Narcan to someone experiencing a different type of medical emergency unrelated to opioids will not do any harm.
Bear in mind that Narcan is not the cure to opioid poisoning—it merely buys time for emergency services to arrive and transport the person to the hospital where they will require further treatment. Narcan is simply sprayed up either nostril, begins working in 1 to 3 minutes, and its “pausing” effect lasts 30 to 90 minutes. It can also be administered as many times as needed until help arrives.
That being said, knowing the signs of opioid poisoning can help you identify the need for Narcan more confidently. According to the Substance Abuse and Mental Health Services Administration, symptoms of opioid overdose/poisoning include:
- Face is extremely pale and/or feels clammy to the touch
- Body goes limp
- Unable to wake up or respond
- Fingernails or lips are a purple or blue color
- Vomiting or gurgling noises
- Breathing or heart rate slows or stops
- Pupils are extremely small or pinpoint
Why is Narcan/Naloxone Needed?
The opioid epidemic has been a serious public health crisis in the United States since the late 1990s when pharmaceutical companies began aggressively promoting and advertising prescription opioids for the treatment of pain.
Unfortunately, opioids are one of the most addictive substances on earth, kicking off the first wave of the opioid crisis. Things would only worsen in the second wave of the 2010s as synthetic (lab-made) opioids like heroin, fentanyl, and methadone started becoming more popular. The problem with synthetic opioids is that they can be tens or hundreds of times more potent than non-synthetic opioids like morphine or codeine. For example, fentanyl is around 50 to 100 times more potent than morphine—just 2 milligrams is a potentially lethal dose.
And with higher potency comes more opioid-related deaths.
 US opioid deaths from 1999 to 2022.
US opioid deaths from 1999 to 2022.
(Courtesy of the National Institute on Drug Abuse (NIDA))
Since 1999, rates of opioid-related deaths have risen almost every year. According to the Centers for Disease Control and Prevention (CDC), more than 560,000 people have died from opioid poisoning since 1999. Things seemed to worsen during the pandemic, with 49,860 US opioid deaths in 2019, 68,360 in 2020, 80,411 in 2021, and 81,806 in 2022. The estimated cost of the opioid epidemic is reported to be a trillion dollars a year.
Sadly, the judgment and stigma around addiction and substance use disorder remain a serious obstacle in discussions of harm reduction measures like Narcan/Naloxone. Substance use disorder is a mental health disorder that causes an individual to experience intense cravings and behavioral changes around substances. Opioid use disorder, in particular, can be challenging to treat, and the road to recovery may include relapses and stumbles along the way. But recovery is possible with the right treatment and support.
However, not all who experience opioid poisoning have opioid use disorder or a drug problem at all.
The problem is contamination and street opioids. Illicit drug manufacturers are secretly adding synthetic opioids, namely illegally made fentanyl, to counterfeit pills of non-opioid drugs to make them “stronger.” In fact, the Drug Enforcement Administration (DEA) reported in 2023 that 7 out of 10 fake prescription pills were found to contain lethal doses of illegally made fentanyl. Some experts even suggest the current number may have grown to 8 or 9 out of 10 pills in 2024.
That means individuals without prior substance problems who are seeking other types of drugs, maybe for the first time or out of crisis, could unknowingly take a lethal dose of an opioid. Perhaps a friend or loved one offers an illegally obtained pill, or someone steals a pill thinking it is a non-opioid drug. These are just a few circumstances in which a person could experience opioid poisoning without a drug addiction problem.
It’s key to remember that prescription opioids are not inherently bad, as medical-use prescription opioids are medically necessary for millions of Americans, including prescription fentanyl. When used as prescribed, many people safely take opioids for pain and will not develop opioid use disorder. However, some people are pre-disposed to patterns of addiction and develop opioid use disorder.
No matter their journey through substance use, all humans deserve help when in crisis, which is exactly what PSTA aims to do by stocking Narcan and training staff on its use.
Trouble in Pinellas
Between 2011 and 2022, Florida was number two in the country for opioid-related deaths. And within the state, Pinellas County remains number one. The Pinellas County Opioid Task Force reports that, in 2022, 597 people died of an overdose, with 80% of those deaths due to opioids. The task force estimates that one person died of an overdose or poisoning every 14 hours in Pinellas County.
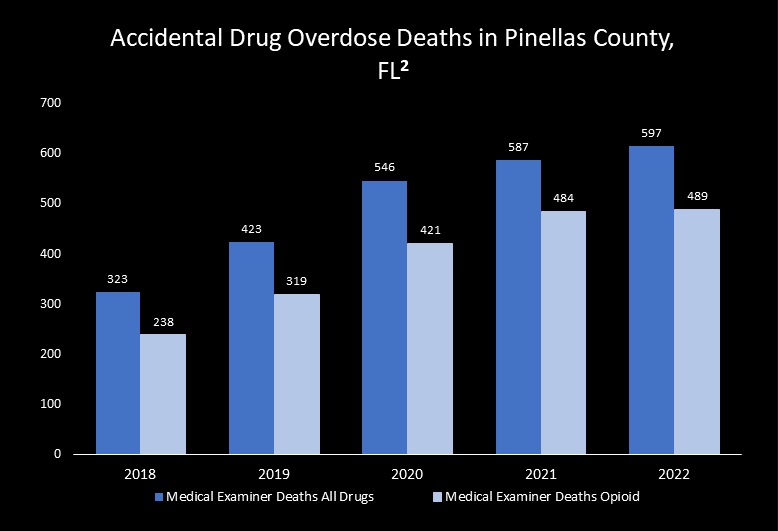 A graph showing all drug overdoses vs. opioid overdoses in Pinellas County from 2018 to 2022
A graph showing all drug overdoses vs. opioid overdoses in Pinellas County from 2018 to 2022
(Courtesy of the Pinellas County Opioid Task Force)
With opioid deaths rising each year, it was clear something needed to be done and fast.
National and State-Wide Initiatives to Help
In 2018, Congress enacted budgets for the State Opioid Response (SOR) and Tribal Opioid Response (TOR), which hoped to increase local access to treatment and intervention for the opioid crisis. The President and his administration have continued to bolster these programs in 2022 and 2024, providing $1.48 billion to states, territories, and the District of Columbia and $63 million to Native Tribes, who have been hit particularly hard by the devastating effects of the opioid crisis.
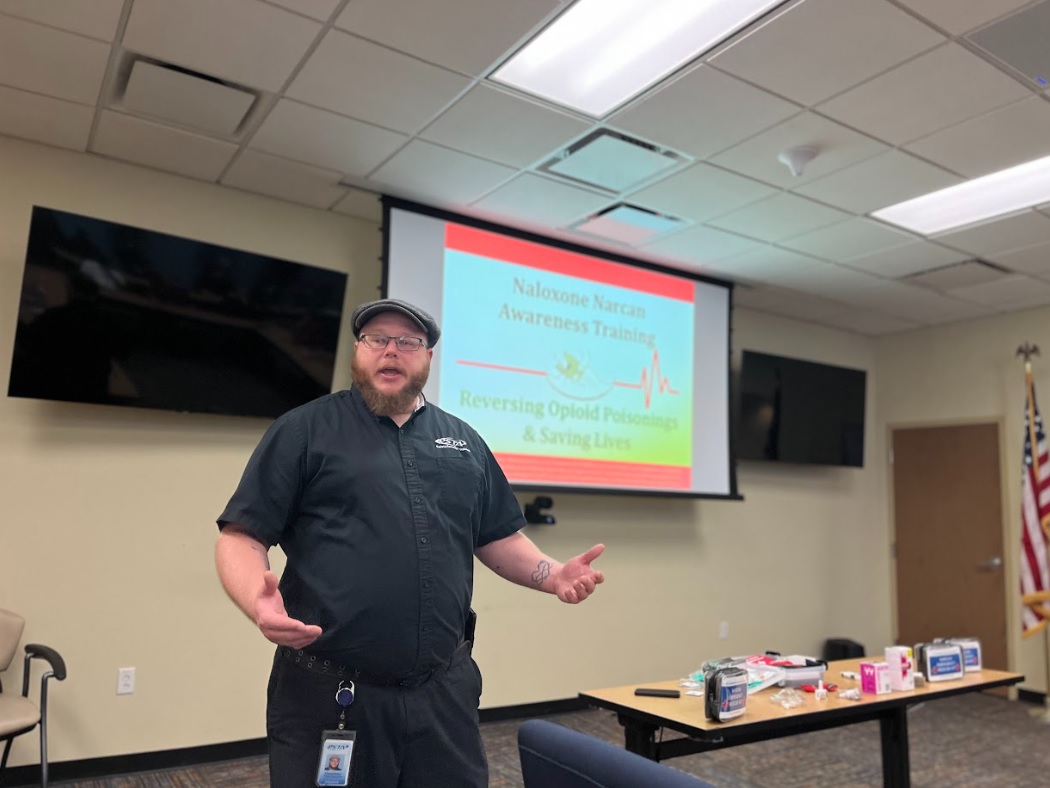
In October 2021, the Pinellas County Board of Commissioners approved a four-year $2 million federal grant from SAMHSA (Substance Abuse and Mental Health Services Administration) to improve opioid poisoning training and response. It would also create the Quick Response Team or QRT, which aims to follow up with patients suspected of having overdosed and who used emergency services for up to 90 days. Through the grant’s yearly funding, Lieutenant Dan Zsido, a retired narcotics investigator with the Pinellas County Sherrif’s office, has partnered with Clearwater’s Recovery Epicenter Foundation to provide organizations with free Narcan/Naloxone training.
 Retired Lieutenant Dan Zsido during the August PSTA Narcan/Naloxone training.
Retired Lieutenant Dan Zsido during the August PSTA Narcan/Naloxone training.
Dan Zsido is also the Training and Education Director of the National Association of Drug Diversion Investigators (NADDI) and assists its Executive Board in the development of substance training and prevention. Thanks to the SAMHSA federal grant, Dan has been able to train over 400 people in Narcan/Naloxone, well over their initial goal of 125.
With the funding in place and resources available, PSTA jumped on the opportunity to do its part in helping our community address the opioid crisis.
PSTA: the First Transit Agency in Florida to Offer Narcan Training
PSTA’s Safety, Security & Training Supervisor, Eddie Kester, has been at the forefront of PSTA’s effort to expand mental health education and resources to help the community. With all the time PSTA employees spend interacting with the public and law enforcement, it was clear that more needed to be done. Eddie called the health department and was put in touch with Dan, who was ready to help PSTA in its new initiative.
 Security & Training Supervisor Eddie Kester during August’s free Narcan/Naloxone training.
Security & Training Supervisor Eddie Kester during August’s free Narcan/Naloxone training.
The very first free Narcan/Naloxone class ever held on the PSTA was in May 2024, and 20 frontline and administrative employees attended. After a successful initial class, plans were made to hold more free classes. The recent class in August 2024 saw 29 more staff attending and officially kicked off PSTA’s Narcan/Naloxone initiative, which has even made national news.
Narcan/Naloxone training has now been incorporated into the onboarding process for new bus operators, with free voluntary classes being made available to administrative staff. In addition, PSTA has now installed Narcan kits in all its terminals, including Grand Central Station, Park Street Terminal, Williams Park, Pinellas Park Transit Center, and PSTA Headquarters.
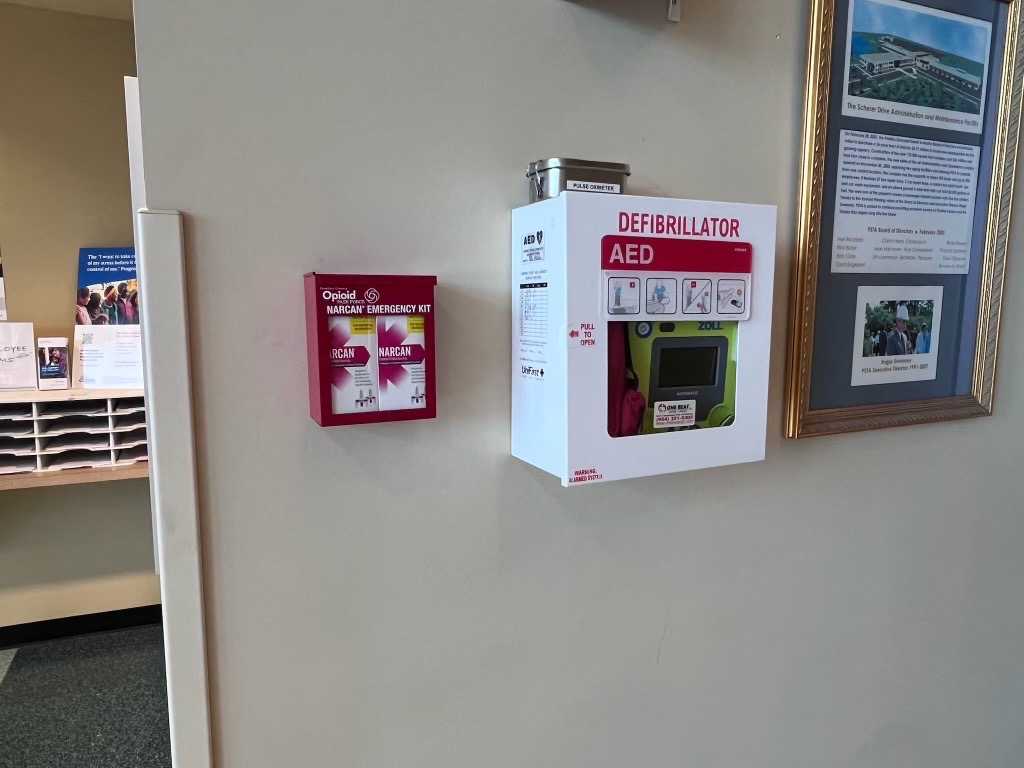 A newly installed Narcan Emergency Kit at PSTA Headquarters.
A newly installed Narcan Emergency Kit at PSTA Headquarters.
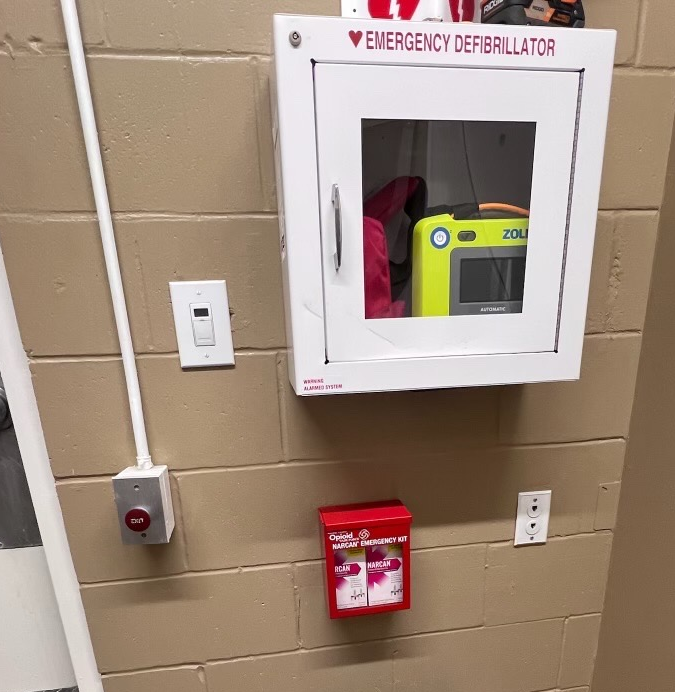
A newly installed Narcan Emergency Kit at Grand Central Station.
This makes PSTA the first transit agency in the state of Florida to offer free Narcan/Naloxone training to staff and to install Narcan kits in all its terminals. The agency will also be the first in the state to have Narcan on all buses—we recently received a shipment of 600 Narcan kits to deploy on all buses in October 2024.

Security & Training Supervisor Eddie Kester and Retired Lieutenant Dan Zsido receiving 600 Narcan kits to go on all buses next month.
The inclusion of Narcan kits on all buses is yet another safety measure that PSTA provides to Pinellas County. All PSTA buses and terminals are part of the Safe Place® program for kids and teens in crisis, a national designation that requires organizations to meet strict requirements and complete specialized training.
PSTA is ready to step up for the community and ensure frontline staff have the tools and confidence to intervene when a community member is in crisis. We’re excited to pave the way for Narcan/Naxolone training in Florida and hope other agencies will join in on this life-saving effort.
Sources
“BCC Approves Grant to Continue Fight Against Opioid Overdoses.” Pinellas County, 12 Oct. 2021, pinellas.gov/news/bcc-approves-grant-to-continue-fight-against-opioid-overdoses/.
“Biden-Harris Administration Awards More Than $1.6 Billion in Funds for Communities Addressing Addiction and Overdose Crises.” Substance Abuse and Mental Health Services Administration, 23 Sept. 2022, www.samhsa.gov/newsroom/press-announcements/20220923/biden-harris-administration-awards-funds-communities-addressing-addiction-overdose-crises.
“DOH-Pinellas Joins Statewide Naloxone Expansion Initiative Targeting Substance Abuse Deaths.” Naloxone Expansion Initiative | Florida Department of Health in Pinellas, 2 Nov. 2022, pinellas.floridahealth.gov/newsroom/2022/11/naloxone-newsroom.html.
“Drug Overdose Deaths: Facts and Figures.” National Institute on Drug Abuse, U.S. Department of Health and Human Services, 22 Aug. 2024, nida.nih.gov/research-topics/trends-statistics/overdose-death-rates.
“FDA Approves First Over-the-Counter Naloxone Nasal Spray.” U.S. Food and Drug Administration, FDA, 29 Mar. 2023, www.fda.gov/news-events/press-announcements/fda-approves-first-over-counter-naloxone-nasal-spray.
“One Pill Can Kill.” DEA, 2023, www.dea.gov/onepill.
“The Opioid Epidemic in Pinellas County.” Pinellas County Opioid Task Force, Esri, 8 Nov. 2023, storymaps.arcgis.com/stories/57761bafd0aa459697ac4ebaf4aecb4f.
“Opioid Overdose Prevention in Tribal Communities.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 30 Jan. 2024, www.cdc.gov/injury/budget-funding/opioid-overdose-prevention-in-tribal-communities.html.
“Opioid Overdose.” Substance Abuse and Mental Health Services Administration, 29 Mar. 2024, www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/opioid-overdose.